Explore how generative AI in healthcare is transforming medical treatments, patient care, diagnostics, applications, and future potential.

Prithvi Bharadwaj
Updated on
December 26, 2025 at 11:27 AM
Healthcare is under constant pressure: rising patient demand, growing costs, and complex clinical decision-making. Traditional digital tools help, but they often automate only routine workflows. Generative AI (GenAI) changes that equation by enabling machines not only to process data but to create new insights, treatment pathways, and even candidate drugs.
From accelerating drug discovery to improving diagnostic imaging, GenAI is already shaping how care is delivered. Analysts estimate the global generative AI in healthcare market could reach $22 billion by 2032, growing at more than 30% annually.
In this blog, we’ll explore how generative AI works in healthcare, its current applications, impact on medical treatments, benefits and risks, and what the future of medicine may look like with GenAI at its core.
Key Takeaways
Generative AI in healthcare is accelerating drug discovery, enhancing diagnostics, and transforming patient engagement—moving from theory to enterprise-scale impact.
Key benefits: faster innovation, lower costs, more accurate diagnoses, personalized treatments, and expanded healthcare access.
Challenges: data privacy, clinical validation, bias, and regulatory gaps—requiring governance, explainability, and human oversight.
The future of health using generative AI will be multimodal, preventive, and globally accessible, with AI acting as a trusted co-pilot for clinicians.
How Generative AI Works in a Medical/Clinical Context
Generative AI in healthcare builds on the same architectures behind large language and multimodal models, but it is trained and validated with domain-specific clinical, biomedical, and imaging data. The difference lies in how it is adapted to regulatory, ethical, and safety-critical environments.
Core Components in a Healthcare Setting
Data Sources: Medical records, diagnostic imaging, genomics, clinical trial data, and biomedical research.
Model Training: Models are fine-tuned on curated, de-identified datasets to minimize bias and protect patient privacy.
Clinical Workflow Integration: GenAI outputs are embedded into electronic health records (EHRs), radiology platforms, and research pipelines to support clinicians in real time.
Validation & Safety: Tools undergo validation studies, often in partnership with hospitals, to prove accuracy, reliability, and compliance with FDA or EMA guidelines.
Human-in-the-Loop Oversight: Critical for clinical adoption—AI may suggest treatment options, but physicians retain ultimate decision-making authority.
By combining large-scale data with clinical oversight, generative AI shifts from being an experimental tool to a trusted co-pilot in healthcare decision-making.
Current Applications of Generative AI in Healthcare
Generative AI is already moving from research labs to hospitals, pharmaceutical pipelines, and patient-facing tools. Its applications span clinical, operational, and research domains:
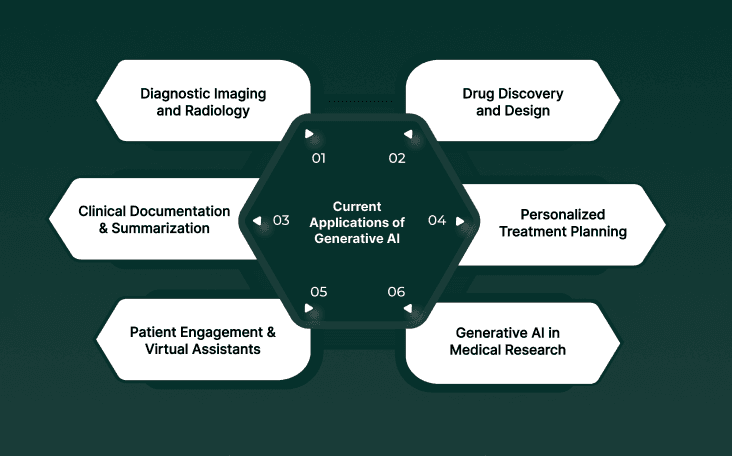
1. Diagnostic Imaging and Radiology
Generative AI enhances medical imaging by filling gaps in incomplete scans, generating higher-resolution images, and assisting radiologists in detecting anomalies. For instance, models can create synthetic MRI or CT images to augment limited datasets, improving diagnostic accuracy.
2. Drug Discovery and Design
Generative AI is already helping pharma companies reduce drug discovery timelines significantly — in some AI-driven discovery platforms, early candidate identification has dropped from years to 12-18 months, and in published work novel small-molecule hits have been discovered in just 30 days from target selection.
3. Clinical Documentation and Summarization
Doctors spend a significant portion of their day on administrative tasks. Generative AI reduces this burden by auto-generating patient notes, summarizing EHR data, and drafting discharge summaries—freeing clinicians to spend more time with patients.
4. Personalized Treatment Planning
By analyzing patient-specific genomic, lifestyle, and clinical data, GenAI helps craft personalized treatment options. For oncology, this means identifying therapies most likely to work for a given tumor profile.
5. Patient Engagement and Virtual Health Assistants
Conversational AI, powered by generative models, is being deployed as virtual nurses or digital health assistants—answering questions, reminding patients about medications, and triaging symptoms before escalation to clinicians.
6. Generative AI in Medical Research
Researchers are using GenAI to generate hypotheses, simulate trial scenarios, and analyze vast biomedical literature. This accelerates insights while reducing manual effort.
Together, these applications illustrate how generative AI is becoming embedded in every layer of healthcare—from labs and clinics to patient homes.
Impact of Generative AI on Medical Treatments
Generative AI is not only improving efficiency in healthcare operations—it’s actively reshaping how medical treatments are developed, delivered, and monitored.
1. Faster Drug Development and Clinical Trials
GenAI helps pharmaceutical companies move from target identification to preclinical candidates far more quickly. By generating and simulating molecular structures, it reduces the time needed to identify viable compounds. This means new treatments can reach patients years earlier than traditional pipelines allow.
2. Personalized and Precision Medicine
Instead of standard “one-size-fits-all” treatments, generative models analyze genomic, imaging, and lifestyle data to propose therapies tailored to individual patients. In oncology, for instance, this can result in customized cancer treatment protocols designed for a patient’s tumor profile, improving both survival rates and quality of life.
3. Enhanced Clinical Decision Support
Generative AI enables treatment simulations, allowing clinicians to test various options virtually before deciding on the best course of care. For complex conditions like autoimmune disorders, this reduces guesswork and supports evidence-based decision-making.
4. Reducing Physician Burden
By automating documentation and synthesizing research, GenAI frees clinicians from repetitive tasks. This indirect impact on treatments matters: more clinician time translates into better patient interaction, more accurate diagnoses, and safer care delivery.
5. Expanding Access to Care
Virtual assistants and multilingual conversational AI are lowering barriers for patients in underserved or remote regions. By triaging symptoms and offering initial guidance, these tools extend access to basic care where specialists are scarce.
Generative AI’s impact on medical treatments is profound: faster therapies, more precise interventions, and expanded access to care. While still in its early stages, the trajectory is clear—AI is shifting from supportive to transformative in the treatment journey.
Benefits of Generative AI in Healthcare
The adoption of generative AI is not just a technological shift—it’s delivering tangible improvements in healthcare outcomes and operations. Here are the most significant benefits:
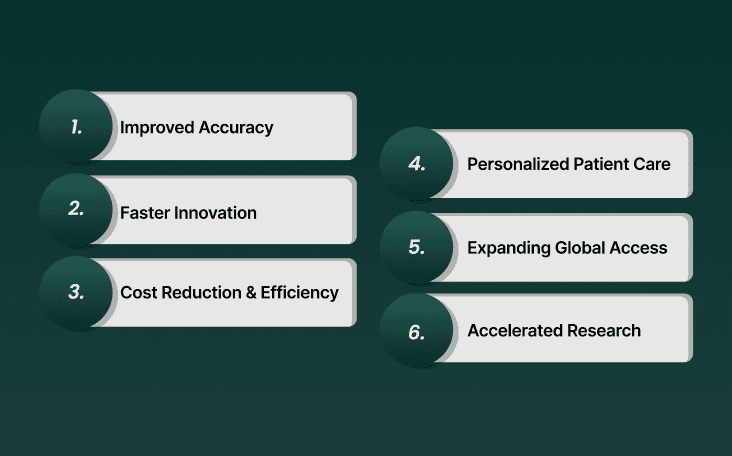
1. Improved Diagnostic Accuracy
By enhancing imaging, analyzing complex datasets, and providing clinical decision support, generative AI helps reduce misdiagnoses. For example, AI-assisted radiology tools can highlight subtle anomalies in scans that human eyes might overlook.
2. Faster Innovation in Drug Discovery
Traditional R&D cycles average 10–15 years and cost billions of dollars. Generative AI shortens early-stage discovery by simulating molecules and predicting efficacy, enabling new therapies to move into clinical trials much faster.
3. Cost Reduction and Efficiency
Automation of clinical documentation, research synthesis, and administrative tasks reduces overhead for hospitals and pharmaceutical companies. In pharma, generative AI could cut drug discovery costs by up to 70%.
4. Personalized Patient Care
By leveraging patient-specific genomic and clinical data, GenAI enables tailored therapies, leading to better outcomes and fewer adverse reactions. This shifts medicine from reactive to truly precision-driven.
5. Expanding Global Access to Healthcare
Virtual assistants and multilingual AI tools extend services to underserved regions. Patients gain 24/7 access to information and triage support, helping reduce the burden on already stretched healthcare systems.
6. Accelerated Research and Insights
Generative AI can scan vast biomedical literature, generate hypotheses, and even simulate trial scenarios. This accelerates research, improves trial design, and helps clinicians stay updated without being overwhelmed.
In short, the benefits of generative AI in healthcare are multifold: better outcomes, faster treatments, reduced costs, and broader access. For enterprises and health systems, these advantages translate into higher efficiency, improved patient trust, and competitive differentiation.
Challenges, Risks, and Ethical Considerations
While the benefits of generative AI in healthcare are compelling, adoption comes with serious challenges. For enterprises and health systems, addressing these risks is non-negotiable.
1. Data Privacy and Security
Healthcare data is highly sensitive. Training generative models on clinical records, imaging, or genomics introduces risks around patient confidentiality. Strict adherence to HIPAA, GDPR, and other data regulations is essential.
Mitigation: Use de-identified datasets, secure storage, and deploy models in on-premises or VPC environments where required.
2. Clinical Validation and Safety
Generative AI can sometimes “hallucinate”—producing outputs that look convincing but are clinically inaccurate. In medicine, this could have life-threatening consequences.
Mitigation: Require clinical trials and peer-reviewed validation before deploying models in patient care. Always keep physicians in the loop.
3. Bias and Fairness
If models are trained on incomplete or biased datasets, they may deliver unequal results across demographics (e.g., underdiagnosing conditions in minority groups).
Mitigation: Regular bias audits, diverse training datasets, and transparent reporting of model limitations.
4. Regulatory and Ethical Oversight
Healthcare is highly regulated, but current frameworks don’t yet fully cover generative AI. The FDA and EMA are still developing guidance on AI/ML-based medical devices.
Mitigation: Enterprises should align early with evolving regulatory frameworks and build explainability and audit trails into their solutions.
5. Integration Into Clinical Workflows
Even the best AI is useless if it doesn’t fit into the daily practice of clinicians. Poorly integrated tools can slow workflows or create mistrust among staff.
Mitigation: Co-design systems with physicians and nurses, integrate into EHRs seamlessly, and ensure minimal disruption to existing processes.
Generative AI in healthcare must be safe, fair, explainable, and integrated. Without these foundations, it risks eroding trust among both clinicians and patients.
Future of Health Using Generative AI
Generative AI in healthcare is still in its early stages, but its trajectory is clear. The future will bring more personalized, proactive, and accessible care, enabled by advanced AI systems that can process multimodal data and integrate seamlessly into medical workflows.
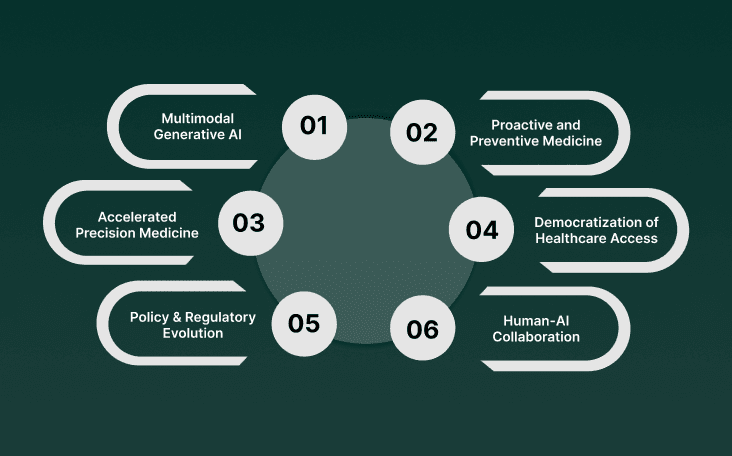
1. Multimodal Generative AI for Comprehensive Care
Future models won’t just process text or images—they’ll analyze medical imaging, genomics, lab results, and patient histories simultaneously. This multimodal intelligence will enable clinicians to see a complete, real-time picture of patient health.
2. Proactive and Preventive Medicine
Instead of waiting for patients to show symptoms, GenAI will help predict risks before they manifest. For example, AI could analyze subtle biomarkers in imaging or genetics to suggest early interventions, shifting healthcare from reactive treatment to preventive care.
3. Accelerated Precision Medicine
GenAI will advance precision medicine by designing therapies tailored to the molecular and genetic profile of each individual patient. In oncology, this means real-time identification of drug combinations most likely to succeed for a given tumor profile.
4. Democratization of Healthcare Access
With multilingual, voice-enabled AI assistants, patients in remote or underserved regions will gain access to guidance and triage support. This could dramatically expand healthcare reach without requiring proportional increases in medical staff.
5. Policy and Regulatory Evolution
Regulators such as the FDA and EMA are expected to publish new frameworks specifically for generative AI in medicine. These will likely address explainability, clinical validation, and data governance—creating a safer path for widespread adoption.
6. Human-AI Collaboration in Everyday Clinical Practice
The future is not about replacing doctors. Instead, AI will act as a clinical co-pilot, providing insights, automating documentation, and surfacing treatment options—while clinicians maintain authority and trust with patients.
The future of health using generative AI will be defined by a blend of science, technology, and policy, creating a healthcare system that is more precise, efficient, and globally accessible.
How to Safely Adopt Generative AI in Healthcare
Adopting generative AI in healthcare isn’t just a technology decision—it’s a matter of patient safety, compliance, and trust. Enterprises and health systems must follow structured best practices to ensure safe and effective deployment.
1. Start with Clinical Validation
Pilot generative AI tools in low-risk, high-volume areas (e.g., documentation, summarization) before moving to diagnostic or treatment use cases.
Require peer-reviewed studies and clinical trials to validate accuracy, safety, and reproducibility.
2. Establish Strong Data Governance
Use de-identified and anonymized datasets during model training.
Define policies for data retention, access control, and audit logging to meet HIPAA, GDPR, and regional compliance standards.
3. Design for Human-in-the-Loop Oversight
Keep physicians and clinicians in ultimate control of patient care decisions.
Implement escalation protocols where AI outputs are flagged for human review.
4. Prioritize Explainability and Transparency
Generative models must provide traceability of recommendations (why a treatment suggestion was made).
Transparent reporting builds trust among clinicians and patients.
5. Vendor Selection Criteria
When choosing a healthcare AI partner, look for:
Regulatory alignment with FDA, EMA, or national authorities.
Security and deployment options (on-premises or VPC for sensitive environments).
Track record in healthcare with published validations or peer-reviewed collaborations.
6. Scale Through Phased Rollouts
Phase 1 (0–6 months): Non-clinical use cases like summarization and administration.
Phase 2 (6–12 months): Research and diagnostic support tools.
Phase 3 (12–24 months): Clinically validated treatment-planning and patient-facing applications.
By approaching adoption in phases—with validation, governance, and oversight—enterprises can scale GenAI in healthcare without compromising safety or trust.
Conclusion
Generative AI is no longer just an emerging technology—it’s becoming a core enabler of modern healthcare. From drug discovery and diagnostic imaging to clinical documentation and patient engagement, its applications are already showing measurable impact. The benefits of generative AI in healthcare—faster innovation, cost savings, and more personalized treatments—are too significant to ignore.
At the same time, challenges around data privacy, clinical validation, and regulatory compliance mean healthcare organizations must adopt GenAI with careful governance. The future of health using generative AI will depend on striking the right balance between innovation and safety, ensuring that AI augments rather than replaces clinical expertise.
How Smallest.ai Can Help Accelerate GenAI in Healthcare
At Smallest.ai, we specialize in building the infrastructure that makes real-time, safe, and scalable AI systems possible. For healthcare, this means:
Low-latency interactions: Sub-100ms performance for natural, human-like voice and chat experiences in patient-facing applications.
Multilingual engagement: Powered by Lightning-v2 multilingual TTS, enabling inclusive patient communication across languages and dialects.
Enterprise-grade compliance: On-premises and VPC deployment options that meet HIPAA, GDPR, and SOC 2 requirements.
Seamless integration: APIs and SDKs that connect easily with EHRs, CRMs, and clinical systems.
With Smallest.ai, healthcare enterprises can safely deploy generative AI in clinical support, patient engagement, and operational workflows—without compromising on compliance or trust.
Ready to explore how generative AI can transform healthcare in your organization? Visit Smallest.ai Healthcare Solutions to learn more.
FAQs on Generative AI in Healthcare
1. What medical fields benefit most from generative AI?
Generative AI is showing strong results in radiology, oncology, drug discovery, clinical documentation, and patient engagement, with more fields expected to follow.
2. Can generative AI replace doctors?
No. Generative AI is designed as a clinical support tool—providing insights, documentation, and simulations—while physicians retain decision-making authority.
3. How is patient privacy protected when using generative AI?
By using de-identified data, secure deployments (on-prem/VPC), and encryption, healthcare organizations can comply with HIPAA, GDPR, and other privacy laws.
4. What are the risks of deploying generative AI in clinical settings?
Risks include hallucinations, bias, privacy breaches, and workflow disruptions. These must be mitigated with validation studies, bias audits, governance, and human oversight.
5. Is there regulatory approval for generative AI tools yet?
Some AI-driven healthcare tools are already FDA- or EMA-approved, but specific guidance for generative AI is still evolving. Enterprises should monitor new frameworks closely.
6. How can smaller hospitals or clinics adopt generative AI safely?
Start with low-risk pilots like documentation support, partner with vendors offering compliance-ready solutions, and scale gradually once results and safety are validated.


